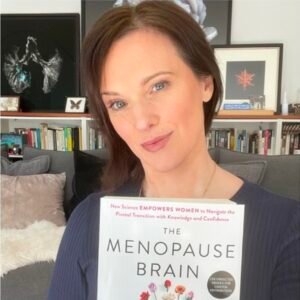
Prof. Lisa Mosconi of neurology: “Menopause is a Brain Renewal Project.

The menstrual cycle of a woman ends at menopause. However, in addition to its effects on the body, the fall in estrogen hormone levels also has an effect on the brain, with symptoms beginning around the age of 47 and continuing for four to eight years. Lisa Mosconi looks into this phenomenon. Her most recent book, “The Menopause Brain,” delves into the brain-inclusive care alternatives for menopausal women as well as the neurological symptoms of the transition and new cognitive abilities that support it. At Weill Cornell Medicine in New York City, Mosconi, an associate professor of neurology and radiology, is 46 years old. She oversees the Women’s Brain Initiative and an Alzheimer’s preventive initiative in association with NewYork-Presbyterian Hospital.
One trending topic is menopause! What contributions does your book make?
from a neuroscientific angle. Furthermore, it’s a facet of menopause that is either disregarded or not specifically mentioned. Although the hot flush is widely acknowledged as a menopausal sign, few doctors associate it with other neurological problems. Nonetheless, our brains and our ovaries are physically connected, and our brains react to the hormones—including estrogen—that our ovaries make. Moreover, our brains must continue to communicate even after our ovaries stop working. Any disturbance to our brain can result in problems. “You’re not losing your mind, rest assured, I’m here to reassure you!”
Which are the most common brain ailments that affect women? And why do they occur?
Hot flashes, nocturnal sweats, trouble sleeping, depression, reduced libido, low energy, and cognitive fog are typical brain symptoms. The end of perimenopause, which occurs when a woman’s menstrual cycle stops for longer than six months, and the early postmenopause are the times when symptoms related to the brain peak.
The reasons of these symptoms are yet unknown to us because the brain is a complicated organ. An essential component is the hypothalamus, which controls body temperature. Rich in estrogen receptors, it is the hub of the interaction between the brain and the ovaries. Hot flashes and night sweats start when estrogen levels start to fluctuate, which occurs during the perimenopause. The hypothalamus interprets conflicting signals and is unable to appropriately regulate body temperature.
You also claim that the brain changes with menopause. In what way?
We see changes in the brain’s structure, connection, and energy production (which decreases but stabilizes in later years or even returns for some) using brain imaging and other methods. Furthermore, the border where symptoms are most acute is where the most alterations in the brain take place.
Menopause, in my opinion, is a project of brain regeneration. There are numerous neural connections in the brain that trace back to the ovaries, but many of these connections become unnecessary and can be broken at menopause. And this causes alterations in the brain that can show up as weaknesses (around this point, we also witness the onset of Alzheimer’s disease in certain women). But in order for a woman to proceed onto her next stage of life, which can nonetheless be just as productive even in the absence of reproduction, the brain must be able to rewire itself. The menopause adaption process and brain reset appear to be two distinct processes (for many people, their symptoms gradually go away), at which point it’s time to rewire and take on new challenges.
What abilities may menopausal women anticipate as a result of this rewiring?

Improved emotional regulation, to start. Globally, menopausal women frequently express feeling more certain, at ease with their identity, and at ease in their own skin than they did previously. The brain’s emotional core, the amygdala, has been demonstrated from a neurological standpoint to selectively become dramatically down-regulated during the menopausal years. It becomes less sensitive to unpleasant or upsetting events in your life. More emotional stability is the outcome, and emotional stability is linked to higher levels of life satisfaction. An increase in empathy is also linked to menopause.
What causes women to experience menopause from an evolutionary standpoint? It is helpful to consider the grandmother hypothesis, which contends that women continue to live longer after menopause because they assist in raising their grandchildren. However, is this theory supported by evidence?
I believe that the speed of our research has to quicken! The grandmother hypothesis makes sense to me, and if women are needed to fulfill that role in life after reproduction, menopause may assist prepare women’s brains for that future. Undoubtedly, our findings make me think that not all menopause-related alterations are negative and harmful. Furthermore, the grandmother is aware of the importance of elder women; after all, very little in nature happens by chance.
Hormone Replacement Therapy (HRT) has a controversial reputation and entails giving women oral doses of either progesterone or estrogen alone to raise hormone levels and help with menopausal symptoms. Is this a wise decision?
It’s a practical choice for a lot of women, and some professional bodies have recently changed their policies to support its application. Nowadays, most healthy women under 60 years old or within ten years after their last menstrual cycle are seen to be safe using it. Professional societies say there is little chance of breast cancer. However, because of the risk of recurrence, HRT is not advised for women who have a personal history of breast cancer. Additionally, most people agree that if HRT is useful, it doesn’t always make sense to stop treatment for women over 60.
Commencing this endeavor at a later stage in one’s life is typically not recommended, as it may potentially correlate with a heightened susceptibility to heart disease, stroke, blood clots, and psychological challenges, among various other concerns.
Although HRT hasn’t been approved for any cognitive problems, it is known to be used off-label for troublesome sleep and moderate depressive symptoms associated with perimenopause. Research on HRT’s potential for brain fog is still continuing.
HRT is undoubtedly not a panacea. It doesn’t operate the same for everyone, nor does it address every problem. Other possibilities include vitamins, behavioral approaches, lifestyle changes, some non-hormonal medicines, and temporary estrogen (for addressing vaginal symptoms of menopause). It is imperative that women possess complete information and base their selections on their risk tolerance and concerns.
Women are twice as likely as males to get Alzheimer’s disease later in life, and there appears to be a connection with hormone replacement therapy. Should women start taking hormone replacement therapy as a preventative measure against Alzheimer’s disease?
My research shows that hormone variations during hormone replacement therapy cause women with disorders (such a family history or genetic markers) to display symptoms of Alzheimer’s. It’s not clear if this holds true for women who have no propensity, but it’s still important to note. It is noteworthy that although every woman experiences menopause, only 20% of them go on to get Alzheimer’s disease. Menopause may weaken the brain, but it is not a direct cause of Alzheimer’s.
At this time, HRT is not advised as a stand-alone treatment for Alzheimer’s disease. Even though there are interesting findings suggesting that it may have preventive properties, additional research is necessary and is currently being conducted. It is thought that HRT may help prevent Alzheimer’s if you are taking it for other symptoms.
Do you have any particular recommendations for preventing things from getting worse, considering that menopause symptoms might affect the onset and intensity of menopausal symptoms?
A plant-based, well-balanced diet that emphasizes whole foods, cuts out on processed foods and refined sugars, and is abundant in antioxidants and fiber—nutrients that are critical for hormone health. Frequent exercise is essential for hormones, the ovaries, and the brain. It also helps you sleep better at night and manage stress. Furthermore, avoid harmful things whenever you can. We are aware that smoking exacerbates symptoms and quickens menopause. Do substances that mess with hormones act in the same way? Although the relationship isn’t entirely understood, we do know that they disrupt the balance of hormones throughout life. In this way, I am now readying myself for the menopause transition.
You contend that managing hot flashes might be made easier by adopting a positive outlook about menopause! It’s difficult to stay optimistic even when hot flashes are excruciating!
Not easy, but necessary. Menopause isn’t as taboo in some countries as it is in ours, and women there usually report milder symptoms. Although it’s complicated, the intellect is strong. Although the symptoms are difficult, in the end, they’re just one more obstacle in life that we must overcome. In general, adopting this mentality is a valuable life lesson.